The Trend of Clinically Diagnosed STI Syndromes and their Determinants Among Female Sex Workers Reached by HIV Prevention Interventions in Tamil Nadu, South India Between 2006 – 2010 Saravanamurthy P. Sakthivel*, Periasamy Mahalingam, Joseph D. Williams
Voluntary Health Services, Chennai, India
*Corresponding author: Saravanamurthy P. Sakthivel
Citation: Sakthivel SP, Mahalingam P, Williams JD (2020) The Trend of Clinically Diagnosed STI Syndromes and Their Determinants Among Female Sex Workers Reached by HIV Prevention Interventions in Tamil Nadu, South India Between 2006 – 2010. Sci Academique 1(1): 40-46.
Received date: 11 December, 2020; Accepted date: 29 December, 2020; Publication date: 31 December, 2020
Abstract
Sexually Transmitted Infections (STIs) prevalence trend indicates the effectiveness of Human Immunodeficiency Virus (HIV) prevention interventions. STI clinical intervention is one of the HIV prevention strategies among various high-risk populations including Female Sex Workers (FSWs). In Tamil Nadu, along with Government supported STI clinics, Tamil Nadu AIDS Initiative-Voluntary Health Services (TAI-VHS, an HIV/AIDS prevention project funded by Bill and Melinda Gates Foundation in Tamil Nadu) established STI clinics beginning 2004, to reach Female and Male Sex Workers (F/MSWs). Systematic analysis and publication of STI clinical data in India was limited due to various reasons. This article analyses the STI clinical data between 2005-2010 recorded in Computerised Management Information System (CMIS) of TAI-VHS program in the year 2011 as part of impact evaluation. These monthly aggregated data does not possess any personal identifiers, ensured as part of data preparation. Trends of STI clinical syndromes, condom distribution, paid peer educators, new STI consultations, and STI clinic establishment was performed. STI interventions were scaled-up in the first two years. The program recorded decreased the STIs clinical syndromes with consistent syndromic management across these five years, with gradual increase in the number of new STI clinics, extensive distribution of condoms, and the role of peer education.
Keywords: Female Sex Workers; STI; HIV; Tamil Nadu; Syndromes
Key Message: Rapid service establishment and sustaining STI service is the key factors of the BMJF funded TAI-VHS STI intervention among FSWs in Tamil Nadu
Introduction
Tamil Nadu is the first Indian state, diagnosed with Human Immunodeficiency Virus (HIV) among Female Sex Workers (FSWs) in the year 1986 [1], followed by the formation of the first State AIDS Cell in India [2]. Targeted Interventions (TIs) among FSWs in Tamil Nadu was first implemented in the year 1995 [2] and the intervention strategies have evolved which included a shift in strategy to syndrome diagnosis and treatment. AIDS Prevention And Control (APAC) – the USAID project in Tamil Nadu conducted a community based study among FSWs in the years 1998 [3] and 2003 [4] to understand and track the trend of STIs.
Sexually Transmitted Infections (STIs) is one of the factors that increase the vulnerability of any population for new HIV infections. This synergy between STIs and HIV was well established by many studies [5,6]. Due to this synergistic effect, the management of STIs became one of the main strategies in HIV/AIDS interventions. Management of STIs in Tamil Nadu, has been done through the state government supported 156 STI clinics, spreads over 32 districts in Government hospitals, Government medical colleges, and Corporation clinics. In addition to these 156 STI clinics, HIV/AIDS interventions, established and supported STI clinics for -high-risk groups (HRG) including Female Sex Workers (FSWs).
Data from these STI clinics could be studied, for the pattern of STIs in the state and district, but it was not much explored. But there were several studies in India and Tamil Nadu, which specifically documented the prevalence of STIs at various points of time and different sub-population [7-9]. These studies supported tracking of the trend of STIs in Tamil Nadu guiding the program designers and policymakers.
In Tamil Nadu, the HIV/AIDS – Targeted Intervention (TI) programs were funded by the Government agency (Tamil Nadu State AIDS Control Society (TANSACS) since 1988, bilateral funded agency APAC – USAID since 1992, and by private donor agency (Tamil Nadu AIDS Initiative (TAI) – Bill and Melinda Gates Initiative (BMGF)) since 2004. In 2006, 30 districts in Tamil Nadu were divided among the three agencies to avoid and/or minimize duplication of services and/or duplication of key population. TAI Initiative implemented TI programs across 12 districts – Coimbatore, Dharmapuri, Dindigul, Erode, Krishnagiri, Madurai, Namakkal, Salem, Tanjore, Theni, Thiruvallur, and Vellore. Out of these 12 districts, except Tanjore and Dindigul, all the other 10 districts were categorized as high prevalence districts (Category A) by NACO [10].
Considering the synergy between the STIs and HIV epidemics (Rothenberg et.al, 2000), and the limited usage of data from Non-Government STI clinics as evidence, the present study had been proposed. This study aims to understand the trends of STI syndromes and the factors driving the syndromes. These findings would possibly inform future programmatic interventions about the role of different determinants. Hence a retrospective analysis was conducted with STI clinic data on services provided to FSWs in TAI-funded districts.
Objective: To describe the trends of clinically diagnosed STI syndromes among FSWs in Tamil Nadu accessing STI services from TAI implemented HIV prevention program and to understand the role of service provisions among the same population.
* A district is a subunit of a state.
Material and Methods
Study Design: This is a retrospective longitudinal analysis of secondary data of STI clinical syndromes. The study considered data from all the 12 districts, where HIV prevention program had STI clinical intervention and systematically maintains the data from these intervention districts. The twelve intervention districts are (1) Coimbatore, (2) Dharmapuri, (3) Dindigul, (4) Erode, (5) Krishnagiri, (6) Madurai, (7) Namakkal, (8) Salem, (9) Tanjore, (10) Theni, (11) Thiruvallur and (12) Vellore.
This trend analysis was carried out in the year 2011, as part of an HIV impact evaluation project based on the data available from the Targeted Intervention (TI) program (funded by TAI – BMGF) available with Avahan-CMIS (Computerised Management Information System) for the period between 2005-2010. This TI program reached female sex workers in twelve districts of Tamil Nadu. The services provided through this project include STI clinical services, condom distribution, peer education, community mobilization, and formation of self-help groups, sensitization, and advocacy programs. The STI clinical services, includes, syphilis testing and syndromic management of STIs. The systematic data flow of the variables from the implementing partners at the district to the CMIS at the national level is presented in figure 1.
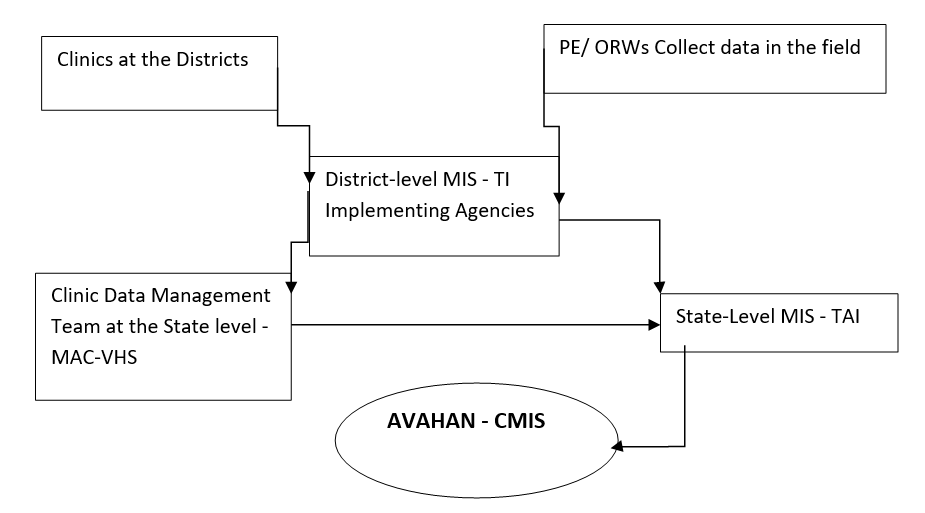
*PE/ ORW-Peer Educator/ Outreach Worker; MIS – Monitoring Information System; TI-Targeted Intervention; MAC-VHS –M.A. Chidambaram-Voluntary Health Services; TAI-Tamil Nadu AIDS Initiative
Figure 1: Data Flow in Avahan Implemented TAI Program in Tamil Nadu.
Data flow from the primary source to CMIS (Figure 1): The field level staffs, including peer educators (PE) and Outreach Workers (ORWs) as part of field level intervention, collect data and refer the appropriate individuals for STI clinical services. The data recorded by the outreach staff reach the district MIS, in addition to the data reported from STI clinics. Every month, these districts’ data are reviewed, approved, and, updated in the State level MIS. Once the State level MIS is reviewed and approved, it finally reaches national level MIS established by the Avahan program of BMGF.
The variables considered for this trend analyses include,
- STI clinics: Number of Clinics established by TAI program,
- Estimated target group: The process of estimating the size of any population, in this case, it is the estimation of FSWs (Table 1).
- Peer educators: Number of individuals selected from FSWs community, based on their willingness to educate their peers on STIs and HIV/AIDS,
- Condom distributed: Number of condoms distributed by the project through various sources including peer educators, outreach workers, and drop-in-center,
- New STI consultancy: Number of FSWs visiting the STI clinic for the first time in the reporting month
|
Districts |
Range of Estimated FSW population (2005 – 2010) |
Districts |
Range of Estimated FSW population (2005 – 2010) |
|
Coimbatore |
1216 – 2000 |
Namakkal |
1200 – 1778 |
|
Dharmapuri |
2786 – 3000 |
Salem |
3000 – 5100 |
|
Dindigul |
1167 – 2614 |
Tanjore |
933 – 1506 |
|
Erode |
1200 – 1642 |
Theni |
1200 – 1911 |
|
Krishnagiri |
3144 – 3500 |
Thiruvallur |
Data not available |
|
Madurai |
3722 – 7000 |
Vellore |
1500 – 2576 |
Table I: Estimated number of FSWs in Districts.
Key STI syndromes were taken for analyses, which includes, (1) Asymptomatic: Women with no complaints of STIs and no signs of STIs detected on examination, (2) Vaginal/ Cervical discharge (VCD): Women complaining of vaginal discharge and/or cervical discharge detected on speculum examination, (3) Genital Ulcer Disease (GUD) – Herpetic / Non-herpetic: Women with genital or anorectal blisters (vesicles) with history of recurrence / Single or multiple and painless or painful ulcer(s) and(4) Lower Abdominal Pain (LAP) / Pelvic-inflammatory Disease (PID): Women with pain/tenderness in the lower abdomen and cervical motion tenderness detected on internal (bimanual) examination.
STI Consultations: The number of STI consultations provided to the key population and non-key populations (regular partners/others) during the reporting period. The total number of consultations is reported and not the number of individuals.
Data Analysis: Trends of STI syndromes were computed year-wise along with condom distribution along with nunmber of peer educators. Besides, number of STI clinics were established, and ‘FSW had STI consultations’ was also observed.
Results
Data available from the Avahan CMIS, of eleven TAI districts in Tamil Nadu between 2005 – 2010 were analyzed for the trends of clinically diagnosed STI syndromes. Table I presents the minimum and maximum range on estimated FSWs in each district, based on which TI was planned. The highest estimates of FSWs were in two districts; Salem and Madurai (> 5000), while the least estimate was in the Tanjore district. During the time of the establishment of TI, Tiruvallur district was not part of the targeted districts, hence estimates of FSW in Tiruvallur district was not available.
Considering the estimated key population, services were established. 15 STI clinics were established in the year 2005 and gradually scaled up to 17 clinics in the year 2008 (Figure 2). Further figure 2 provides information about a significant decline of 76% in new STI consultations from 2006 to 2010.
Figure 3 provides a comparison between the number and types of clinically diagnosed STI syndromes among FSWs (bar graph), condom distribution, and the number of peer educators (PEs). The syndromes presented in the graph, especially VCD shows a consistent decline from the second year 8925 cases (2006) to the last reported the year 2409 (2010). Condom distribution had been at a consistent level, except for the first and last year of the study period. The number of paid peer eductors also shows a significant increase of 1233 in the first three years and decline in the last three years to up to 726.
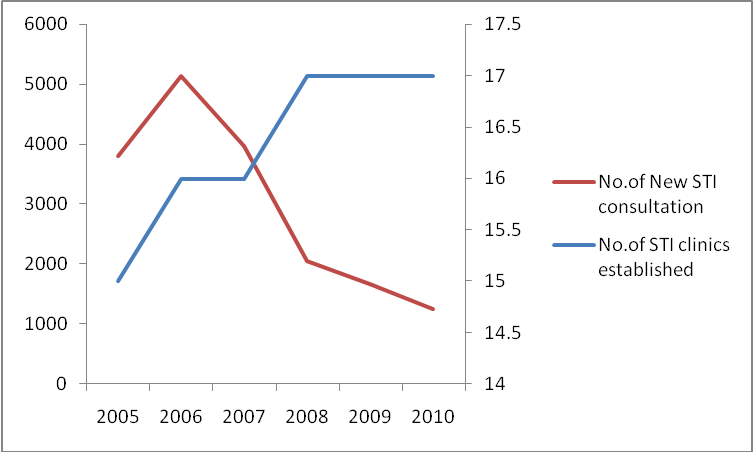
Figure 2: No.of STI clinics Established and New STI Consultation over six-year period.
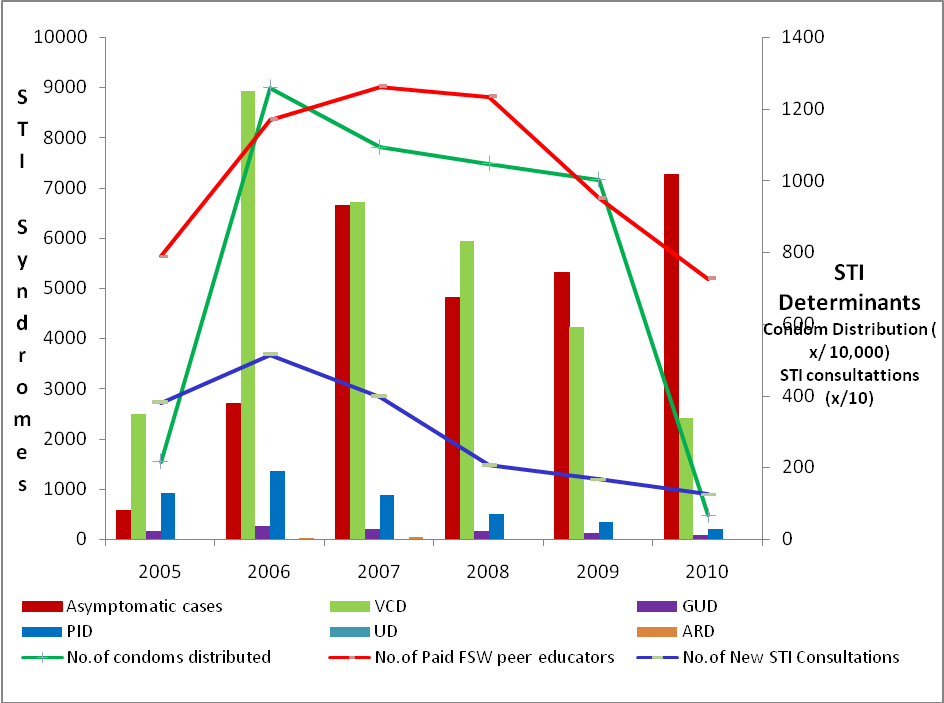
Figure 3: Trend of clinical diagnosed STI syndromes among FSW accessing services against the Determinants (2005 – 2010).
Discussion
A review article commented on STIs among FSWs in India would rise to 6.87 million in 2005 from 2.49 million in 1999. To avoid this scenario, early diagnosis, appropriate treatment, and rigorous follow-up was recommended [11]. TAI with this evidence supported the rapid establishment of STI clinics, sustained coverage of the FSW population, bridged the key population with STI clinics with the help of field staff (peer educators/outreach workers), provided STI/HIV prevention messages, and enabled access for STI/HIV preventive services. This was evident in the first two years of the program, where there was an increasing trend of new STI consultations, which explains the extensive reach of the FSWs through peer educators. These Peer educators have educated the target population about the STI syndromes and the necessity of treating the same at the STI clinics available in the intervention sites. Further, the sustained service provision through the STI clinics & outreach programs has resulted in the decline of new STI consultations during 2005 – 2010.
The reduction in new STI syndromes was due to the syndromic treatment approach followed in the intervention clinics and that could have been coupled by the increased condom access either through peer educators, ORWs, clinics, and condom depot.
Figure 3 shows a clinically significant increase in the number of asymptomatic cases and a significant decline in the symptomatic STI cases. This reduction in symptomatic cases could be contributed to the success of STI syndromic management in large populations. In a developing country like India, the advantage of syndromic management is highly appreciated and acknowledged among public health programs [11]. In general, this decline in clinically symptomatic STIs could be contributed to the scenario of declining bacterial STIs than viral STIs. This decline of bacterial STIs than viral STIs among various populations is well established by different cross-sectional studies showing laboratory evidence [12-14].
The other aspect which is attributed to the decline in the new STI consultation is the effective free condom distribution during the first five years. The association between condom use and STIs is established in a recent meta-analysis of studies around the world [15]. A comparison between the number of free condoms distributed and the number of peer educators shows that there is a significant decline in the condom distribution when the peer educators were less in number. But other compounding factors are – Voluntary condom procurement of clients by themselves, Voluntary condom procurement from traditional outlets (pharmacies), and non-traditional outlets (other shops) by the FSWs. The availability of condoms from the private market has also enabled FSWs to procure the condom without depending on the free condom supply from the TI projects. Availability of various patterns and flavours of condoms at an affordable price could be the reason for the non-preference of the TI project supplied free condoms.
Limitation
This paper analysed cumulative data available from Targeted interventions, hence, statistical significance and association of the STI downward trend could not be analyzed.
Conclusion
The impact of rapid establishment of STI clinics, scaled-up coverage of key populations, the role of outreach staff, and consistent condom use in reducing the STI trend among FSWs in Tamil Nadu should be studied with a more robust study design. This downward trend of diagnosis of STI syndromes could be a transient phase, hence ensuring sustained access to STI services for this key population is recommended to maximize and extend the benefit of Targeted interventions in Tamil Nadu.
References
- Simoes EA BP, John TJ, Nirmala S, Solomon S, Lakshminarayana CS, et al. (1987) Evidence of HTLV-III infection in Prostitutes in Tamil Nadu. Indian Journal of Medical Research 85: 335-338.
- Saravanamurthy PS, Martine Collumbien (2013) HIV/AIDS Epidemic, Prevention Efforts, and the Contextual Factors in Tamil Nadu – A Monograph. Chennai: Voluntary Health Services.
- APAC-VHS. Community Prevalence of Sexually Transmitted Diseases in Tamil Nadu. Chennai, Tamil Nadu: Voluntary Health Services; 1998.
- APAC-VHS. Community Prevalence of Sexually Transmitted Diseases among General Population and High-Risk Groups in Tamil Nadu. Tamil Nadu: Voluntary Health Services; 2003.
- JN W (1992) Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sexually Transmitted Diseases 19: 61-77.
- Mayaud P, McCormick D (2001) Interventions against sexually transmitted infections (STI) to prevent HIV infection. British Medical Bulletin 58: 129-153.
- Ginnela NV, Brahmam VK, Rajkumar H, Rachakulla HK, Kallam S, et al. for the IBBA Study Team. (2008) Sexual practices, HIV, and sexually transmitted infections among self-identified men who have sex with men in four high HIV prevalence states of India. AIDS 22: s45-s57.
- Maharajan MVS, Balasubramanian M, Karunanithy T, Jagadeesan M (2006) A retrospective study of STI patterns and its implications in framing strategies for the state STI control program, Tamil Nadu, India. Paper presented at International Conference on AIDS. Toronto, Canada.
- Saravanamurthy PS, Rajendran P, Miranda PM, Ashok G, Raghavan SS, et al. (2010) A Cross-sectional study of Sexual Practices, Sexually Transmitted Infections, and Human Immunodeficiency Virus among Male-to-Female Transgender People. American Medical Journal 2: 87-93.
- NACO. District Categorization for Priority Attention. New Delhi: National AIDS Control Organization; 2006.
- Vinod K, Sharma SK (2004) Changing patterns of sexually transmitted infections in India. The National Medical Journal of India 17.
- Saravanamurthy PS, Miranda PM, Ashok G, Raghavan SS, Arnsten JH, et al. (2010) A Cross-sectional Study of Sexual Practices, Sexually Transmitted Infections, and Human Immunodeficiency Virus among Male-to-Female Transgender People. American Medical Journal 1: 87-93.
- Panda S, Kumar SM, Saravanamurthy PS, Mahalingam P, Vijayalakshmi A, et al. (2007) Sexually Transmitted Infections and Sexual Practices in injecting drug users and their regular sex partners in Chennai, India. Sexually Transmitted Diseases 34: 250-253.
- Subramanian T, Gupte MD, Paranjapee RS, Brahmam GNV, Ramakrishnan L, et al. for the IBBA study Team. (2008) HIV, Sexually Transmitted Infections and Sexual Behaviour of Male clients of Female Sex Workers in Andhra Pradesh, Tamil Nadu and Maharashtra, India: results of a cross-sectional survey. AIDS 22: S69-S79.
- Scott-Sheldon LA, Hudeo-Medina TB, Warren MR, Johnson BT, Carey MP (2011) Efficacy of Behavioral Interventions to Increase Condom Use and Reduce Sexually Transmitted Infections. Journal of Acquired Immune Deficiency Syndromes 58: 489-498.