Transvaginal Sonographic Diagnosis of an Endometrial Polyp Causing Mechanical Interference to Implantation and Growth of Conceptus in a Young Subfertile Woman with Recurrent Pregnancy Loss Aanchal Gupta*, Naresh Seervi
Department of Diagnostic and Interventional radiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India
*Correspondence to: Aanchal Gupta
Citation: Gupta A, Seervi N (2022) Transvaginal sonographic diagnosis of an endometrial polyp causing mechanical interference to implantation and growth of conceptus in a young subfertile woman with recurrent pregnancy loss. Sci Academique 3(2): 37-43
Received: 13 September, 2022; Accepted: 26 September 2022; Publication: 30 September 2022
Abstract
Endometrial polyps are benign masses and are rarely symptomatic. The most common presentation of endometrial polyps when symptomatic is abnormal uterine bleeding [1]. Often, they are incidentally detected in women being investigated for other entities. A handful of infertility cases are associated with this not so uncommon entity [1]. Various plausible mechanisms such as mechanical hindrance to sperm and ovum transport, generalized inflammation of endometrial cavity and failure of implantation due to space limitation have been proposed [1]. As radiologists, we ought to be familiar with the imaging features of endometrial polyps which can be easily missed/misdiagnosed if not for a high index of suspicion. In this case report, we intend to describe the imaging features of uterine polyps on ultrasound which is a cheap, noninvasive and often the first line of investigation for pre and postmenopausal women.
Keywords: Endometrial polyp; Interrupted mucosa; Feeding vessel; Pedicle artery sign; Saline infusion sonohysterography
Case Report
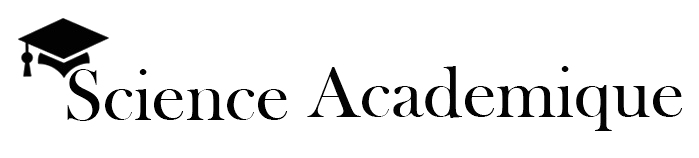
We report a case of a 24-year-old lady who was unable to conceive for a period of 8 years. Infertility workup was negative. In 2018, she conceived, however cardiac activity was not demonstrated in the fetus and eventually medical abortion was performed. Transvaginal sonography was performed for the same at a private center which did not pick up any uterine structural abnormality. In 2021, the patient presented to our emergency department with a 14-week gestation pregnancy with complaints of bleeding per vaginum for 2 days. Antenatal transvaginal ultrasound was performed for confirmation and viability of an intrauterine pregnancy. An intrauterine gestational sac with crown rump length corresponding to 8 weeks 5 days and absent cardiac activity was seen suggesting the diagnosis of missed abortion (Figure 1). Surrounding the gestational sac was fluid with internal echoes suggesting failure of implantation (Figure 2). A well-defined uniformly echogenic pedunculated lesion was seen in the endometrial cavity (Figure 3). As it was traced towards the point of its origin, a focally hypoechoic region was demonstrated interrupting the hyperechoic endometrial lining (Figure 4), classically described as the ‘interrupted mucosa sign’ [2]. On colour doppler image, a single vascular pedicle was demonstrated (Figure 5), known as the ‘pedicle artery sign’ [3]. Based on these classical features the diagnosis of an endometrial polyp was made. It was seen to abut the gestational sac suggesting mechanical hindrance to growth of the embryo (Figure 6). On real time imaging, the endometrial polyp was seen prolapsing from towards the uterine fundus to the lower uterine segment (Figure 7). For better characterization of the endometrial polyp, it has been recommended to distend the uterine cavity with saline (also known as saline infusion sonohysterography) [4,5], however in our case it was unwarranted because the gestational sac and fluid naturally distended the uterine cavity and helped in optimum visualization (Figure 4,6). Figure 8 depicts another case of an endometrial polyp showing a non-gravid uterus with an echogenic lesion in the endometrial cavity showing the classical interrupted mucosa sign (Figure 8A) and the feeding artery sign (Figure 8B).
Uniformly hyperechoic pedunculated lesion with a vascular stalk which showed prolapse on real time images helped us conclusively make the diagnosis of an endometrial polyp as opposed to the close differential of submucosal leiomyoma which more commonly appears as a broad-based round hypoechoic lesion, often with internal cystic areas and without the classical signs namely ‘interrupted mucosa sign’ and ‘pedicle artery sign’ as seen in endometrial polyps. Another differential that was considered was of intrauterine clots, however they are usually more heterogenous in echogenicity and have an ill-defined contour. Retained product of conception was not kept as a differential as intrauterine gestational sac and fetal pole were well visualized.
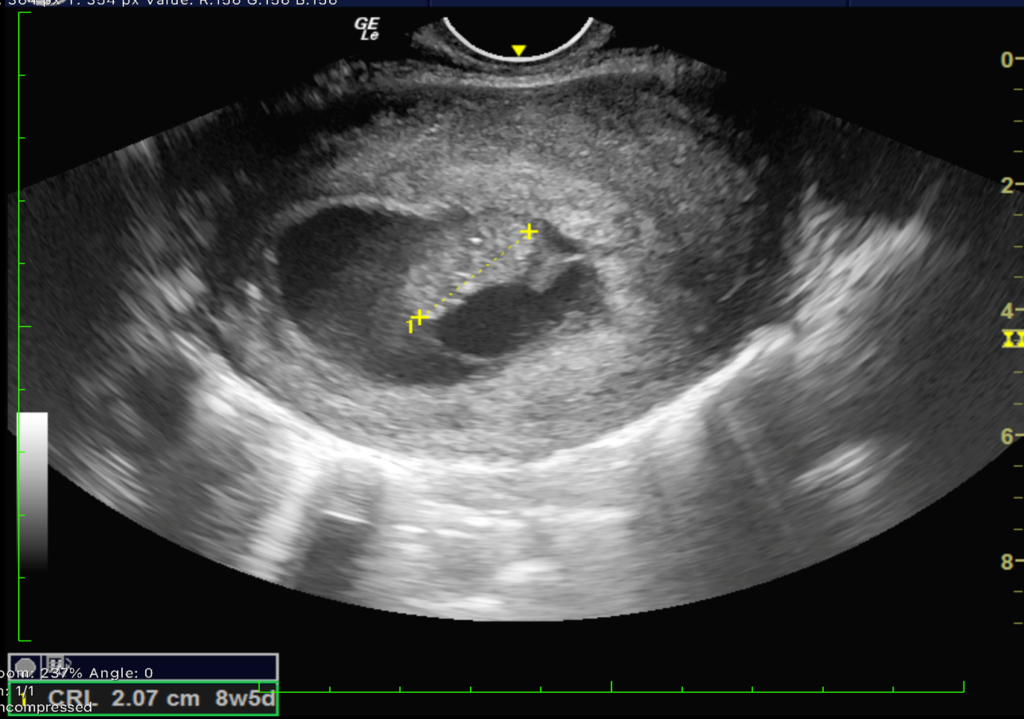
Figure 1. Transvaginal sonography shows an undifferentiated fetal pole with absent cardiac activity corresponding to 8week 5 days in a 14 week gestational pregnancy calculated from last menstrual period.
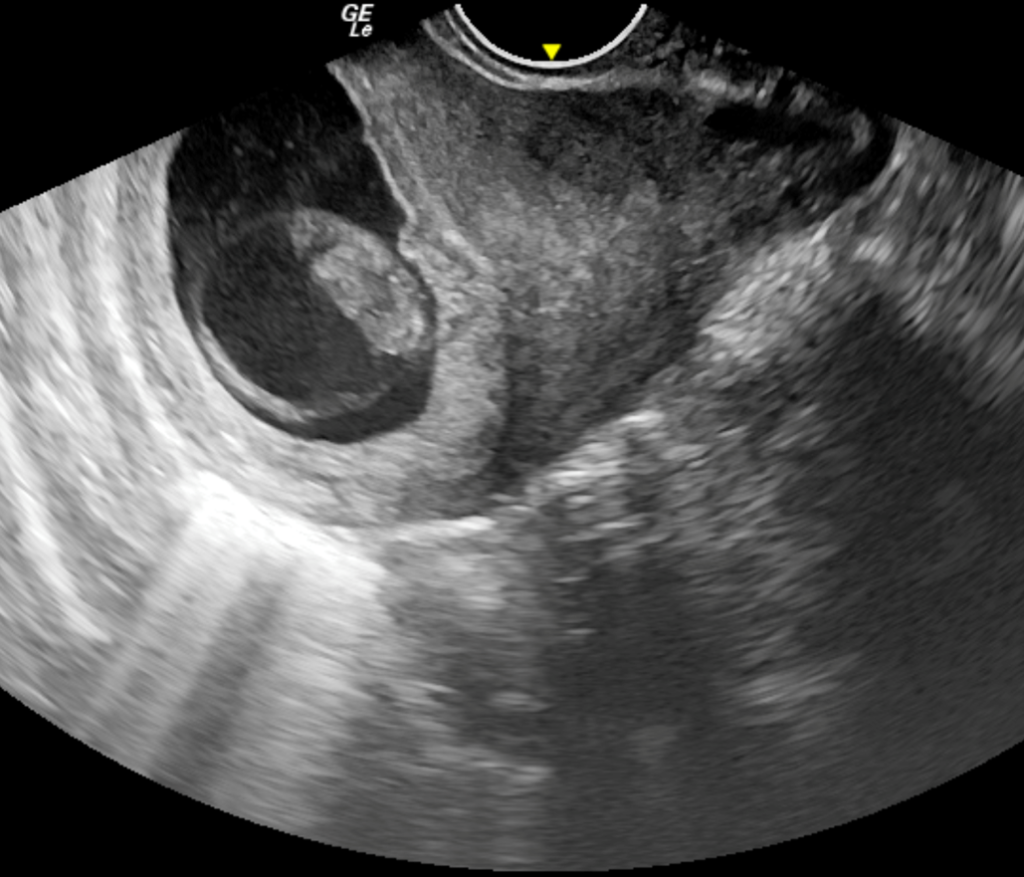
Figure 2. Transvaginal sonography shows a gestational sac within the endometrial cavity without a definite site of implantation. Note the surrounding echogenic fluid.
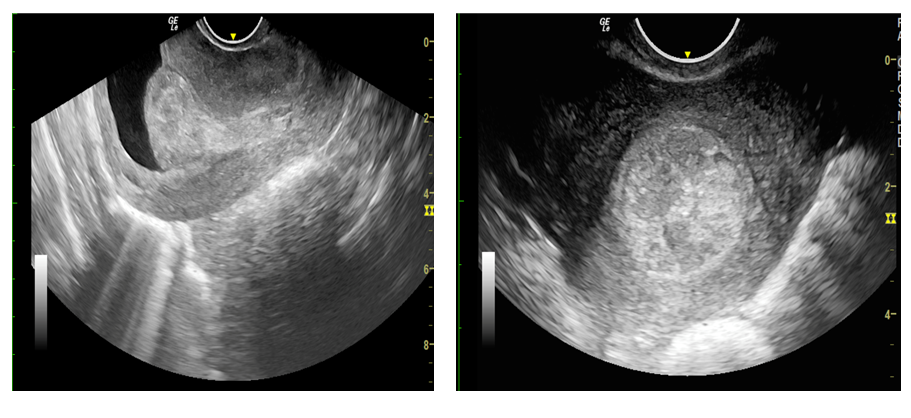
Figure 3: Transvaginal sonography A) Sagittal section B) Axial section show a well defined, well contoured, homogenously hyperechoic lesion in the endometrial cavity with a stalk suggestive of endometrial polyp.
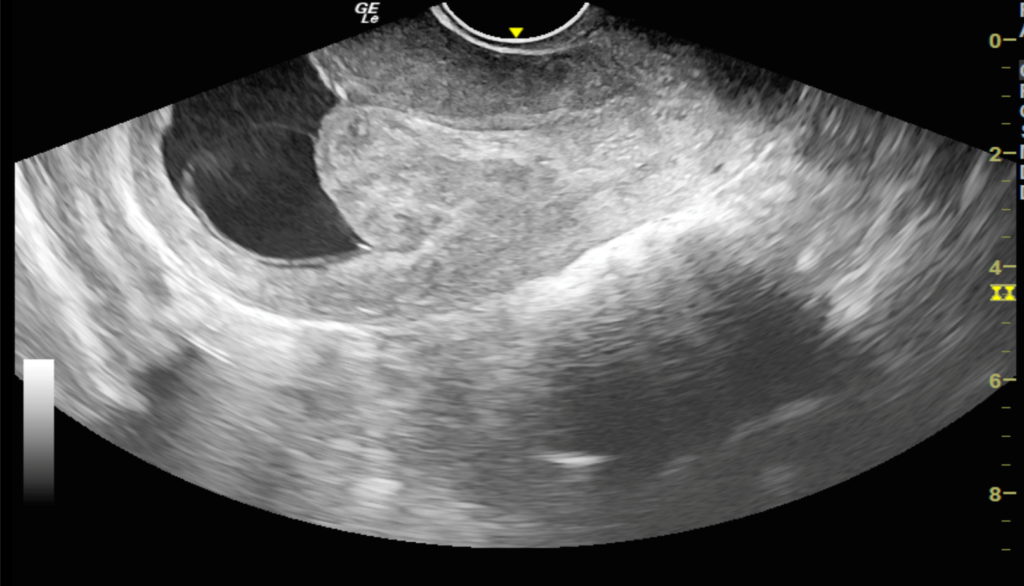
Figure 4: Sagittal section of transvaginal sonography shows a focal hypoechoic region (blue arrow) at the base of polyp which is seen to interrupt the hyperechoic endometrial lining (red arrow), described as the ‘interrupted mucosa sign’.
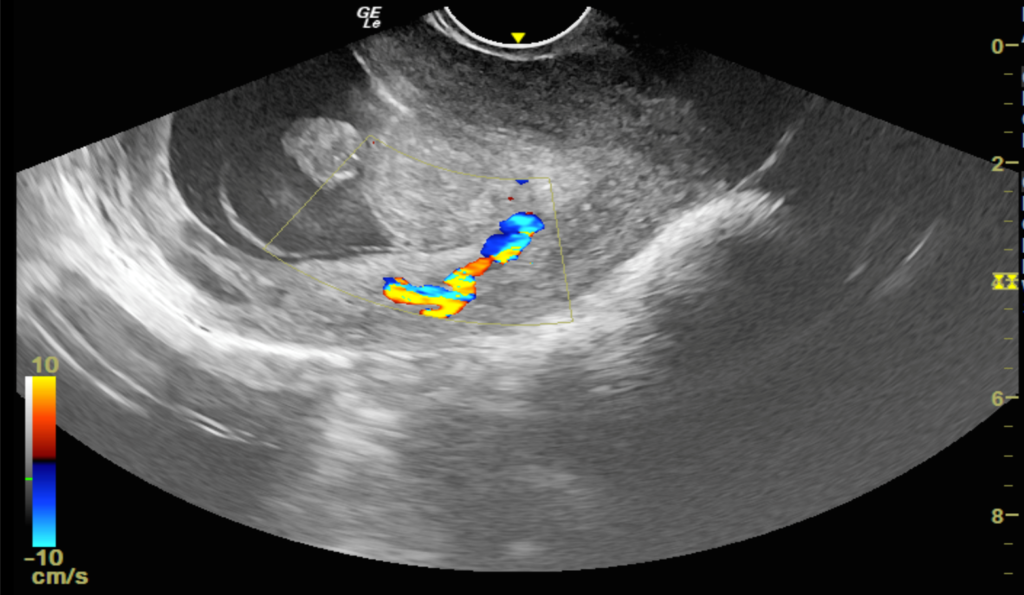
Figure 5: Color doppler images show a single feeding artery supplying the stalk of polyp, described as ‘pedicle artery sign’.
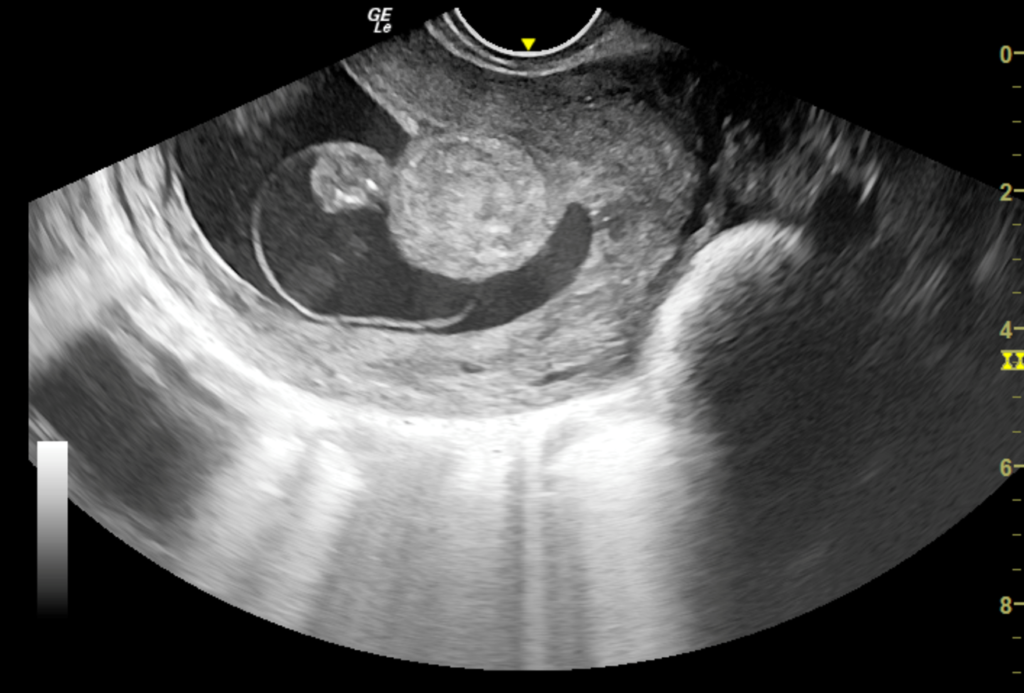
Figure 6: Axial section of transvaginal sonography depicting the mechanical hindrance to implantation and growth of fetus by the well defined polypoidal lesion. Also note the natural distension of endometrial cavity by fluid in gestational sac and endometrial cavity beautifully delineating the polyp margins thus obviating the need for saline infusion in this case.
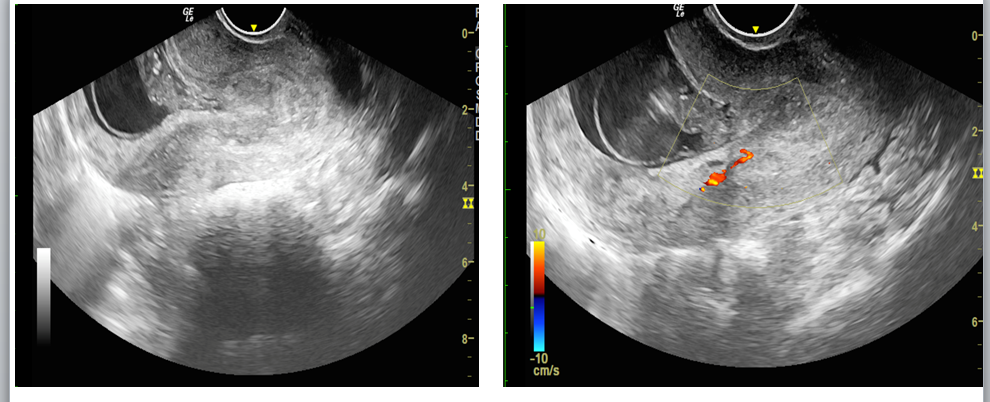
Figure 7: Sagittal sections of transvaginal sonography showing the prolapse of endometrial polyp towards the lower uterine segment. Also note the feeding vessel oriented downwards towards the stalk of polyp.
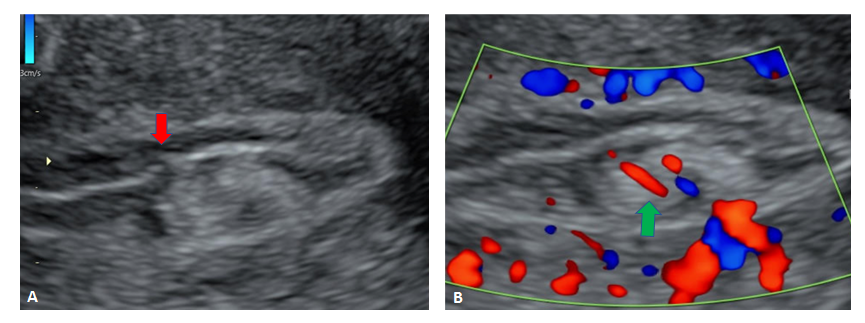
Figure 8: Another case of endometrial polyp showing a non-gravid uterus with an echogenic lesion in the endometrial cavity showing the classical interrupted mucosa sign (Figure 8A, red arrow) and feeding artery sign (Figure 8B, green arrow).
Discussion
Endometrial polyps are benign focal overgrowths of endometrial tissue, often with variable amounts of vascularity and stroma encased by epithelium [2]. They are known to be associated with infertility and recurrent pregnancy loss. This case report is unique as it describes how the diagnosis of an endometrial polyp was established on transvaginal sonography in a young gravid female with history of inability to conceive for about a decade and a previous pregnancy loss.
A well-defined homogeneously hyperechoic mass in the uterine cavity observed by sonohysterography is most suggestive of an endometrial polyp [6,7] as was seen in our case. They can be sessile or pedunculated. The interrupted mucosa sign is a unique sign associated with endometrial polyps with a high predictive value which is identified when the highly echogenic linear interface of the opposing endometrial mucosal surfaces can be followed to a point at which it is focally interrupted [2]. A feeding artery supplying the stalk of polyp affirms the diagnosis of an endometrial polyp [3].
The plausible association of endometrial polyps with infertility can be attributed to a mechanical interference with sperm and embryo transport, impairment of embryo implantation or through intrauterine inflammation or increased production of glycodelin, a glycoprotein shown to inhibit sperm-oocyte binding and NK cell activity [8]. Rackow, et al. in their study established that uteri with endometrial polyps have an altered expression of HOX gene which diminishes the endometrial receptivity at a molecular level. The reduced gene expression of HOXA10 and HOXA11 messenger RNAs influences embryonic and glandular development of uterus and causes a globally diminished endometrial receptivity for fertilization [9]. The physical surface area of the polyp also prevents implantation of the embryo into the endometrium, thus acting as a space occupying lesion [1].
Stamatellos, et al. concluded that irrespective of number and size of polyps, fertility rates were significantly improved in patients who underwent hysteroscopic polypectomy thus negating the long-term belief that small polyps do not adversely affect pregnancy outcomes [10]. Miscarriage rates were found to be higher in polyps >2 cm in size [11].
Hysteroscopic removal remains the mainstay of treatment and is associated with favourable fertility outcomes [9,12].
Conclusion
Endometrial polyps are difficult to diagnose and may remain unidentified especially in infertile females who are otherwise asymptomatic. This case is unique as it depicts the sonographic diagnosis of an indolent endometrial polyp which was undiagnosed for years in a young asymptomatic woman who was unable to conceive for almost a decade and had suffered an early pregnancy loss in the past. Current pregnancy was complicated by the polyp impinging on the gestational sac thus hindering with its proper implantation and growth and subsequent pregnancy loss.
Declaration of patient consent: A written informed consent was obtained from the patient.
Acknowledgement: None
Financial support and sponsorship: None
Conflicts of interest: None
References
- Nijkang NP, Anderson L, Markham R, Manconi F (2019) Endometrial polyps: Pathogenesis, sequelae and treatment. SAGE Open Med 7: 2050312119848247.
- Kamaya A, Yu PC, Lloyd CR, Chen BH, Desser TS, et al. (2016) Sonographic Evaluation for Endometrial Polyps: The Interrupted Mucosa Sign. J Ultrasound Med 35: 2381-2387.
- Timmerman D, Verguts J, Konstantinovic ML, Moerman P, Van Schoubroeck D, et al. (2003) The pedicle artery sign based on sonography with color Doppler imaging can replace second-stage tests in women with abnormal vaginal bleeding. Ultrasound Obstet Gynecol 22: 166-171.
- Fadl SA, Sabry AS, Hippe DS, Al-Obaidli A, Yousef RR, et al. (2018) Diagnosing Polyps on Transvaginal Sonography: Is Sonohysterography Always Necessary? Ultrasound Q. 34: 272-277.
- Jorizzo JR, Chen MY, Riccio GJ (2001) Endometrial polyps: sonohysterographic evaluation. AJR Am J Roentgenol 176: 617-621.
- Tamura-Sadamori R, Emoto M, Naganuma Y, Hachisuga T, Kawarabayashi T (2007) The sonohysterographic difference in submucosal uterine fibroids and endometrial polyps treated by hysteroscopic surgery. J Ultrasound Med 26: 941-946.
- Kupfer MC, Schiller VL, Hansen GC, Tessler FN (1994) Transvaginal sonographic evaluation of endometrial polyps. J Ultrasound Med 13: 535-539.
- Al Chami A, Saridogan E (2017) Endometrial Polyps and Subfertility. J Obstet Gynaecol India 67: 9-14.
- Rackow BW, Jorgensen E, Taylor HS (2011) Endometrial polyps affect uterine receptivity. Fertil Steril 95: 2690-2692.
- Stamatellos I, Apostolides A, Stamatopoulos P, Bontis J (2008) Pregnancy rates after hysteroscopic polypectomy depending on the size or number of the polyps. Arch Gynecol Obstet 277: 395-399.
- Lass A, Williams G, Abusheikha N, Brinsden P (1999) The effect of endometrial polyps on outcomes of in vitro fertilization (IVF) cycles. J Assist Reprod Genet 16: 410-415.
- American Association of Gynecologic Laparoscopists. AAGL practice report: practice guidelines for the diagnosis and management of endometrial polyps. J Minim Invasive Gynecol 19: 3-10.