The Importance of Preoperative Enteral Nutrition in Patients with Malignoma of The Colon Pašić Fuad 1*, Elezović Haris 2, Mehmedović Zlatan1, Jagodić Samed3, Hođić Renata4, Pašić Amela 5
1Surgery Clinic, Tuzla University Clinical Centre, Medical Faculty in Tuzla Bosnia and Herzegovina
2General Hospital Sanski Most, General Surgery Ward Bosnia and Herzegovina
3Urology Clinic, Tuzla University Clinical Centre, Bosnia and Herzegovina
4Neurology Clinic, Tuzla University Clinical Centre, Medical Faculty in Tuzla, Bosnia and Herzegovina
5Clinic for children’s diseases, Tuzla University Clinical Centre, Medical Faculty in Tuzla, Bosnia and Herzegovina
*Correspondence to: Pasic Fuad
Citation: Fuad P, Haris E, Zlatan M, Samed J, Renata H, et al. (2024) The importance of preoperative enteral nutrition in patients with malignoma of the colon. Sci Academique 5(2): 79-88
Received: 26 June, 2024; Accepted: 24 July, 2024; Published: 2 August, 2024
Abstract
Objective: The primary goal of this paper is to indicate that surgical patients with colon malignancy who receive specialized oral nutritional support during the pre-operative period can improve their nutritional status. These measures, consecutively, can reduce consumption of fresh frozen plasma and human albumin but also improve overall results in the post-operative treatment period.
Methods: Three groups of patients were followed with colon malignancy. Two groups received a pre-operative nutritional support preparation of Fresubin 2 x 200 millilitres for 7 and 14 days, respectively, and a third group that did not receive nutritional support.
Results: Our research, although on the preliminary sample, speaks of a clear tendency that subjects who had been on enteral diet for 14 and 7 days, had lower needs for human albumin compared to a group without enteral nutrition. No statistically significant difference was detected in the quantities of distributed SSP (p = 0.62), while there was a marginal signification for ordinated albumin doses.
Conclusion: There is space for continuation of this research by increasing the sample and providing extended time monitoring of the operated patients, all for the benefit of oncological digestive patients.
Introduction
Malnutrition of surgical oncology patients with colon malignancies is common, a ‘side effect’ that to a lesser or greater extent limits outcomes in the treatment of these patients. The problem of tumour cachexia is a “widespread” medical problem worldwide. Some authors mention malnutrition in as many as 85% of hospitalized cancer patients. If we talk specifically about colon cancer, malnutrition occurs in 30-60% of the total number of hospitalized patients. It has been shown that malnutrition is an independent risk factor for increased post-operative morbidity and mortality, and that its presence prolongs the patient’s stay and increases the number of post-operative complications [1,2]. Back in 1936, Studley documented a close relationship between malnutrition and complications in patients who were surgically treated for stomach ulcers. Studies conducted during this period suggest that 33% of patients with a higher weight loss of 20% before surgery died compared to 3.5% of patients with a weight loss of less than 20% [3,4].
Eighty years later, despite the progress of surgical and anaesthesiological techniques, malnutrition persists in surgical patients with gastro-intestinal tumours. It has a relationship with a higher rate of postpartum complications (72% vs 29%) and mortality (23% vs 4%) compared to well-fed or normally fed patients [5].
The paper we wrote gives preliminary answers as to whether optimising oral nutrition in the pre-operative period with specialized supplements can lead to a better overall nutritional status of surgical oncology patients with colon malignancies. This approach, consecutively, should lead to lower hospital consumption of post-operatively fresh frozen plasma and human albumin, but also to better results in the treatment of surgical patients with colon resection. We underline that undernourished, hospitalized surgical patients have significantly worse clinical outcomes in treatment. These include a four-fold higher risk of mortality, a higher risk of surgical complications, more frequent re-admission, prolonged hospitalisation and increased healthcare and treatment costs [6-8]. In the shortest, possible objectives to be achieved with optimisation of pre-operative nutrition in cancer patients are: avoid starvation to maintain protein status, maintain immune, muscle and endocrinological function, and accelerate post-operative recovery [9].
Objective of the Study
Our study aimed to objectively evaluate the impact of optimizing substitute pre-operative specialized nutrition on a preliminary sample of patients with elective resection surgery due to colon cancer.
Inclusion criteria
- Consenting patients with colorectal resection,
- Patients with performed colonoscopy and established PHD diagnosis,
- Abdominal ultrasound,
- Pre-operative CT diagnosis of the abdomen and pelvis with oral and intravenous contrast,
- MRI of the abdomen and pelvis performed for rectal cancer,
- NRS 2002 score of degree of malnutrition determined,
- Full biochemical profile completed.
Exclusion criteria
- Patients operated under emergency protocol,
- Incomplete documentation, or incomplete patient’s documentation.
All patients on the consenting surgical program covered by this clinical study underwent preoperative colon cleansing with antibiotic prophylaxis (cefazolin, metronidazole 2 hours preoperatively 2×1.0). All patients were reviewed and recommended by the Digestive Council of the Tuzla University Clinical Centre for surgical treatment of colon cancer. Using the methodology of random selection, three groups of monitored patients were created at the Digestive Council itself. The first group of patients or 20 of them received a recommendation for one week of preoperative enteral nutrition with the Fresubin preparation dosed twice a day. The second group of patients or 20 of them received a recommendation for preoperative consumption of Fresubin dosed twice a day for two weeks. Thirdly, a group of 28 patients did not receive a recommendation for alternative nutritional support. In both groups consuming the Fresubin preparation, the patients received the maximum recommended daily dose of 2×1 bottle or 2×200 ml of the preparation. The Fresenius Cabi enteral preparation was used. The preparation has different pleasant flavours adapted to make it as pleasant as possible for consumption. As per indication from a medical doctor, it is used as a supplement preparation. Importantly, it is high in protein (milk), vegetable oils (rapeseed oil, sunflower oil), carbohydrates, vitamins, minerals, triglycerides. Most often it is used as dietary supplement. It is recommended to drink the preparation slowly, spread over several hours or throughout the day between meals, not to spoil the appetite and maintain normal food intake. Recommended maximum daily dose is 2 bottles or 400 ml of the preparation. The preparation tastes best when cooled. It can be served warm, heated in the microwave oven (the bottle must be opened beforehand) or it needs to be gently heated in a deep dish with constant stirring.
Results
Our study was conducted in 2023 as a prospective study at the Surgery Clinic, Tuzla University and Clinical Centre, Bosnia and Herzegovina. A total of 68 patients were monitored and analyzed. Three groups of monitored patients were formed. Two groups of 20 (29.4%) were treated with substitute enteral preparations for one and two weeks, respectively, and 28 made up the third group who were not treated with enteral preparations.
| Group | Total | |||||
| Ent. prep. Two weeks | Ent. prep. One week | Without ent. prep. | ||||
| Sex | M | N | 12 | 17 | 21 | 50 |
| % | 24.0% | 34.00% | 42.0% | 100.0% | ||
| F | N | 8 | 3 | 7 | 18 | |
| % | 44.4% | 16.7% | 38.9% | 100.00% | ||
| Total | N | 20 | 20 | 28 | 68 | |
| % | 29.4% | 29.4% | 41.2% | 100.00% | ||
Table 1: Gender breakdown of patients in the analyzed groups.
| Variable | Two weeks | One week | No treatment | p-value |
| Gender (M: %, F: %) | M: 60.0% | M: 85.0% | M: 75.0% | 0.196 |
| F: 40.0% | F: 15.0% | F: 25.0% | ||
| Average age | 66.3 | 67.15 | 65.71 | 0.868 |
| Age – SD | 11.46 | 10.69 | 5.63 | |
| CV Diseases (Yes: %, No: %) | Yes: 80.0% | Yes: 85.0% | Yes: 67.86% | 0.35 |
| No: 20.0% | No: 15.0% | No: 32.14% | ||
| DM (Yes: %, No: %) | Yes: 10.0% | Yes: 20.0% | Yes: 17.86% | 0.66 |
| No: 90.0% | No: 80.0% | No: 82.14% | ||
| Other (Yes: %, No: %) | Yes: 25.0% | Yes: 20.0% | Yes: 25.0% | 0.91 |
| No: 75.0% | No: 80.0% | No: 75.0% | ||
| NRS 2002 – average | 2.45 | 2 | 1.11 | <0.001 |
| NRS 2002 – SD | 1.05 | 0.56 | 1.03 | |
| Day zero erythrocytes – average | 4.44 | 4.23 | 4.35 | 0.62 |
| Day zero erythrocytes – SD | 0.76 | 0.67 | 0.6 | |
| Hgb zero day – average | 127.75 | 121.95 | 126.11 | 0.67 |
| Hgb zero day – SD | 21.87 | 22.04 | 20.46 | |
| Htc zero day – average | 0.38 | 0.37 | 0.38 | 0.71 |
| Htc zero day – SD | 0.06 | 0.06 | 0.06 | |
| On day zero – average | 140.05 | 139.11 | 139.36 | 0.53 |
| On day zero – SD | 3.07 | 2.30 | 2.77 | |
| K zero day – average | 4.24 | 4.13 | 4.24 | 0.66 |
| K zero day – SD | 0.44 | 0.45 | 0.47 |
Table 2: Descriptive comparative presentation of basal features in analyzed patients.
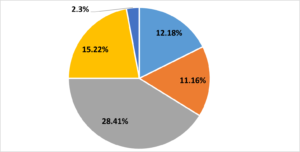
Figure 1: Breakdown of patients by NRS 2002.
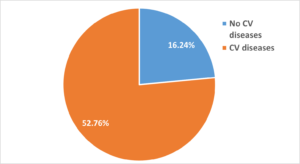
Figure 2: Breakdown of patients by presence of CV diseases
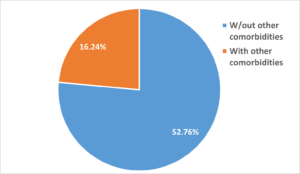
Figure 3: Breakdown of patients by presence of associated diseases.
The results of the survey provided important insights into the effects of enteral nutrition in patients in their perioperative period. It was observed that the length of administered enteral nutrition (one or two weeks) did not significantly affect the key outcomes, namely the length of hospitalization, the occurrence of complications or the need for transfusion. These findings suggest that while enteral nutrition plays an important role in patient recovery, the optimal timing of nutrition may not play a critical role.
The average amount of SSP prescribed to all patients in the total observed sample was 551 ml and ranged from 0 to 1810 ml. The average amount of albumin prescribed was 122 ml and ranged from 0 to 450 ml. Patients also received an average of 0.2 doses of blood, ranging from 0 to 2 doses. No statistically significant difference was detected in the amounts of SSP distributed (p=0.62), while there was a borderline significance for the prescribed doses of albumin (p=0.05) – Figures 5 and 6.
As seen from Figure 6, there was a clear tendency for patients on enteral nutrition for two weeks or one week to have lesser need for albumins compared to the group without enteral nutrition. This was further explored, and found that patients in the group with enteral nutrition for two weeks had an average need of 101 ml of albumin, those in the group who had enteral nutrition for one week had an average need of 107 ml of albumin, while those in the group without enteral nutrition needed an average of 148 ml of human albumin.
Despite the absence of major differences in the average duration of hospitalization and length of stay in the intensive care unit between the study groups, a tendency of reduced need for albumin administration was found in the groups of patients treated with enteral nutrition. This indicates the possible benefit of enteral nutrition in reducing nutritional deficits, which is in line with previous studies that highlighted the importance of adequate nutritional support in the postoperative period.
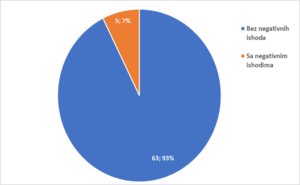
Figure 4: Breakdown of patients by treatment outcomes.
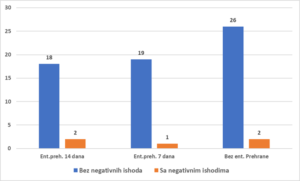
Graph 1: Breakdown of patients by treatment outcomes.
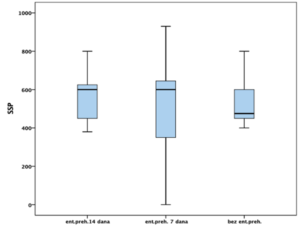
Figure 5: SSP consumption in studied groups.
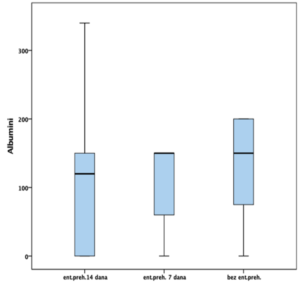
Figure 6: Humane albumin consumption in studied groups.
Discussion
Given that this is virtually the only statistically significant difference between the groups in the NRS 2002 score, this variable in itself is highlighted and imposes the need for further research regarding the impact of nutritional status on final outcomes in the treatment of patients with colon resection procedures, which, as mentioned earlier, are all too often malnourished and with nutritional deficits found. Malnutrition is known to be a predictor of hospitalization costs, increasing costs between 19% and 29% [10].
Nutritional status can play a vital role in recovery and resistance to the possible occurrence of surgical complications following this branch of surgery much like a shadow. Complications in colorectal surgery have occurred throughout the past and are bound to occur in the future as well. Advancements in safe technologies and new surgical modalities in surgical treatment, laparoscopic, that is, robotic oncological colon surgery, have clearly made colon operations safer and with better outcomes. With these technological advances, along with a longer learning curve, technical errors have been minimized. Although visible qualitative advances have been made in this purely operative part of the treatment of patients with colon cancer, unfortunately, extremely malnourished patients still go to operating tables around the world. This is an everyday fact in surgery and oncology, yet to a lesser extent found in highly developed countries.
Conclusion
- A large number of patients with oncological digestive diseases come to the operating table with evident malnutrition.
- The presence of malnutrition can affect recovery and outcomes in the treatment of patients with colon malignancies.
- There is space in pre-operative processing and preparation of these “serious” and difficult patients to come to the operating room with a better nutritional profile and a better overall biological response.
- With diagnostic procedures imperatively important is to detect tumors in earlier stages of the disease, it is not less important to detect nutritional deficiencies in oncology patients in time, properly classify them and start correct them as soon as possible.
- For “our” analysed, diseased patients, a replacement seven-day specialized diet at the full recommended dose of 2 x 200 ml of Fresubin was comparatively costing one bottle 20% of human albumin.
- Economic benefits for patients are not neglected, but also for medical institutions that will consume less fresh frozen plasma and human albumin in the post-operative course of recovery with this approach.
- We can, freely, say that the designed “small pre-op investments” can bring multiple benefits in further treatment, with no observed adverse effects on patients.
- Enhanced Response to Treatment
- Better-nourished patients tend to have an improved response to chemotherapy and radiation therapy. Adequate nutrition can: Enhance the effectiveness of oncological treatments. Reduce the side effects associated with these treatments.
- Quality of Life: Improved nutritional status leads to better physical function and quality of life. Patients experience: Increased strength and energy levels. Better tolerance to treatments and surgical procedures. Overall improved well-being.
It is important to point out once again that in the treatment of these most severe, oncological patients, imperative is, synchronous and timely needs to detect the nutritional deficits that are almost always present in them. With the measures designed, respecting the underlying illness, general and local status of the patient, we believe that we should start correcting all present deficits as soon as possible, even in the pre-operative period. No adverse effects of this approach have been observed, and we have preliminary, clear indications that these measures and procedures can in many ways have positive, beneficial effects on the treatment of these patients.
References
- Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, et al. (2001) Early postoperative enteral nutrition improves gut oxygenation and reduces costs with total parenteral nutrition. Crit Care Med 29: 242-8.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68: 394-424.
- Global Burden of Disease Cancer C, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. (2017) Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 3:524-48.
- Cerantola Y, Grass F, Cristaudi A, Demartines N, Schafer M, et al. (2011) Perioperative Nutrition in Abdominal Surgery. Recommendations and Reality. Gastroenterology Research and Practice: 739347: 8.
- Correia MIDT, Waitzberg DL (2003) The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariante model analysis. Clin Nutr 22: 235-9.
- HO Studley (1936) Percentage of lost weight: a basic indicator of surgical risk in patients with chronic peptic ulcer. J Am Med Assoc 106: 458-460
- Meguid MM, Debonis D, Meguid V, Hill LR, Terz JJ (1988) Complications of abdominal operations due to malignant disease. Am J Surg 156: 341-345.
- Toiyama Y, Okugawa Y, Shimura T, Ide S, Yasuda H, et al. (2020) Neutrophil priming as a risk factor for surgical site infection in patients with colon cancer treated by laparoscopic surgery. BMC Surg 20: 5.
- Tangvik RJ, Tell GS, Eisman JA, et al. (2014) Nutrition strategy: four issues predict morbidity, mortality and health care costs. Clinical Nutrition 33: 634–41.
- Guerra RS, Sousa AS, Fonseca I, et al. (2016) Comparative analysis of malnutrition screening and diagnostic tools as predictors of hospitalization costs. Journal of Human Nutrition and Dietetics 29: 165 – 73.